Periodontal Disease
Diagnosis | Treatment | Maintenance
Diagnosis | Treatment | Maintenance
The word periodontal means “around the tooth”. Periodontal disease attacks the gums and the bone that support the teeth. Plaque is a sticky film of food debris, bacteria, and saliva. If plaque is not removed, it turns into calculus (tartar). When plaque and calculus are not removed, they begin to destroy the gums and bone. Periodontal disease is characterized by red, swollen, and bleeding gums. Four out of five people have periodontal disease and don’t know it! Most people are not aware of it because the disease is usually painless in the early stages. Not only is it the number one reason for tooth loss, research suggests that there may be a link between periodontal disease and other diseases such as, stroke, bacterial pneumonia, diabetes, cardiovascular disease, and increased risk during pregnancy. Researchers are determining if inflammation and bacteria associated with periodontal disease affects these systemic diseases and conditions. Smoking also increases the risk of periodontal disease. Good oral hygiene, a balanced diet, and regular dental visits can help reduce your risk of developing periodontal disease.
Periodontal treatment methods depend upon the type and severity of the disease. Your dentist and dental hygienist will evaluate for periodontal disease and recommend the appropriate treatment. Periodontal disease progresses as the sulcus (pocket or space) between the tooth and gums gets filled with bacteria, plaque, and tartar, causing irritation to the surrounding tissues. When these irritants remain in the pocket space, they can cause damage to the gums and eventually, the bone that supports the teeth! If the disease is caught in the early stages of gingivitis, and no damage has been done, one to two regular cleanings will be recommended. You will also be given instructions on improving your daily oral hygiene habits and having regular dental cleanings. If the disease has progressed to more advanced stages, a special periodontal cleaning called scaling and root planning (deep cleaning) will be recommended. It is usually done one quadrant of the mouth at a time while the area is numb. In this procedure, tartar, plaque, and toxins are removed from above and below the gum line (scaling) and rough spots on root surfaces are made smooth (planning). This procedure helps gum tissue to heal and pockets to shrink. Medications, special medicated mouth rinses, and an electric tooth brush may be recommended to help control infection and healing. If the pockets do not heal after scaling and root planning, periodontal surgery may be needed to reduce pocket depths, making teeth easier to clean. Your dentist may also recommend that you see a Periodontist (specialist of the gums and supporting bone).
Non-Surgical Procedure
Scaling and Root Planing is one of the most effective ways to treat gum disease before it becomes severe. Root planing and scaling cleans between the gums and the teeth down to the roots. Your dentist may need to use a local anesthetic to numb your gums and the roots of your teeth. If anesthesia is used, your lips and gums may remain numb for a few hours. Planing and scaling causes little or no discomfort.
If you maintain good dental care after the procedure, the progression of gum disease should stop. And your gums will heal and become firm and pink again. Non-surgical therapy does have its limitations, however, and when it does not achieve periodontal health, surgery may be indicated to restore periodontal anatomy damaged by periodontal diseases and to facilitate oral hygiene practices.
Surgical Procedure
If you’re diagnosed with periodontal disease, your periodontist may recommend periodontal surgery. Periodontal surgery is necessary when your periodontist determines that the tissue around your teeth is unhealthy and cannot be repaired with non-surgical treatment. Following are the four types of surgical treatments most commonly prescribed:
Your bone and gum tissue should fit snugly around your teeth like a turtleneck around your neck. When you have periodontal disease, this supporting tissue and bone is destroyed, forming “pockets” around the teeth.
Over time, these pockets become deeper, providing a larger space for bacteria to live. As bacteria develop around the teeth, they can accumulate and advance under the gum tissue. These deep pockets collect even more bacteria, resulting in further bone and tissue loss. Eventually, if too much bone is lost, the teeth will need to be extracted.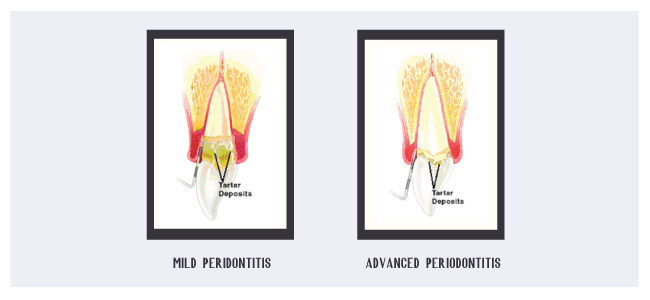 Your periodontist has measured the depth of your pocket(s). A pocket reduction procedure has been recommended because you have pockets that are too deep to clean with daily at-home oral hygiene and a professional care routine.
During this procedure, your periodontist folds back the gum tissue and removes the disease-causing bacteria before securing the tissue into place. In some cases, irregular surfaces of the damaged bone are smoothed to limit areas where disease-causing bacteria can hide. This allows the gum tissue to better reattach to healthy bone.
Your periodontist has measured the depth of your pocket(s). A pocket reduction procedure has been recommended because you have pockets that are too deep to clean with daily at-home oral hygiene and a professional care routine.
During this procedure, your periodontist folds back the gum tissue and removes the disease-causing bacteria before securing the tissue into place. In some cases, irregular surfaces of the damaged bone are smoothed to limit areas where disease-causing bacteria can hide. This allows the gum tissue to better reattach to healthy bone.
Reducing pocket depth and eliminating existing bacteria are important to prevent damage caused by the progression of periodontal disease and to help you maintain a healthy smile. Eliminating bacteria alone may not be sufficient to prevent disease recurrence. Deeper pockets are more difficult for you and your dental care professional to clean, so it’s important for you to reduce them. Reduced pockets and a combination of daily oral hygiene and professional maintenance care increase your chances of keeping your natural teeth – and decrease the chance of serious health problems associated with periodontal disease.
It only takes twenty four hours for plaque that is not removed from your teeth to turn into calculus (tartar)! Daily home cleaning helps control plaque and tartar formation, but those hard to reach areas will always need special attention.
Once your periodontal treatment has been completed, your dentist and dental hygienist will recommend that you have regular maintenance cleanings (periodontal cleanings), usually four times a year. At these cleaning appointments, the pocket depths will be carefully checked to ensure that they are healthy. Plaque and calculus that is difficult for you to remove on a daily basis will be removed from above and below the gum line.
In addition to your periodontal cleaning and evaluation, your appointment will usually include: